Last Friday, two of my patients who had had
DCR (dacryocystorhinostomy) surgery for blocked nasolacrimal ducts returned for removal of the tubes which were inserted to ensure patency of the connection between the tear sac and the nose. The removal involved cutting the tube at the eye level and asked to blow their noses hard to expel the tube.
The first patient was a 50 year-old man who did this without problem.
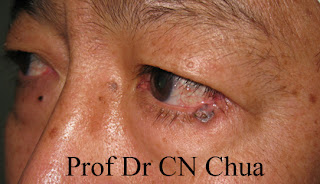
Tube at the level through the holes that drain tear.
The tube was cut at the eye level.
The patient was instructed to blow his nose.
The tube that was blown out of the nose.
The second patient was a 75 year-old woman who had problem blowing her nose. So I attempted to expel the tube by flashing the tear duct. Although she could feel the water running down her throat, the tube was not expelled through the nostril. Consequently, I have to examine her nasal cavity for the missing tube. Unfortunately, the tube could not be found. I suspected the tube might have been flushed into her throat and swallowed. The tube is not toxic and should not cause any untoward effect.
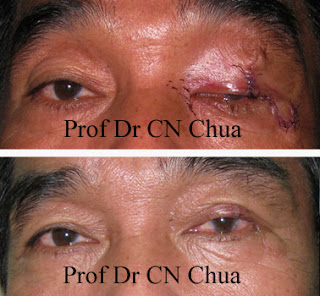
The DCR tube at the eye level.
The tube was cut with a pair of scissors.
The cut tube could now be removed through the nostril.
The nose was inspected for the missing tube.
The arrow indicates the hole created to join the tear sac
to the nose so that the tear can be drained.
Diagram showing where the tube might go.
The blue circle indicates the hole (fistula) created between the tear sac and the nose.The green lines represent the DCR tube. The tube usually came out through the nostril (red arrow) when one blow the nose. The tube might have been swallowed because during flushing in the second patient, the tube might have been pushed into the throat (blue arrow).