Although eyebags may be removed by making an incision below the eyelashes, the disadvantages of this approach are many including:
a. a scar extending along the length of the lower eyelids which may take time to heal
b. longer down time as the approach is associated with more bruising and swelling
c. risk of lower eyelid retraction especially if the skin and muscle are removed.
To avoid these complications, the fat may be removed from behind the eyelids (a transconjunctival approach) in suitable patients.
Julien Bourguet (1876-1952), a French surgeon was the first to introduce transconjunctival blepharoplasty. His results were described and published in 1924 with photographs (see photographs below).
One of the patients of Julien Bourguet who
had had transconjucntival blepharoplasty.
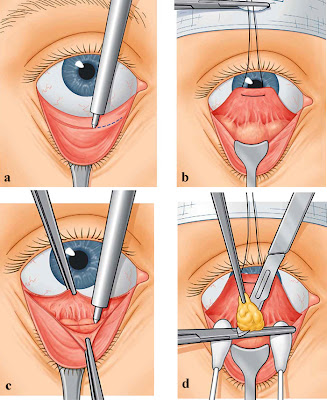
Bourguet's method is still in use and the steps are shown in the diagrams below.
Diagrams showing transconjunctival approach for fat removal.
Transconjunctival approach is used mainly in patients whose main problem is eyebag. This method does not address the problem of loose skin and therefore is not suitable for patients who need skin tightening. Most of my patients having this procedure are patients in their 20s and 30s.
Transconjunctival fat removal at one month post-operative.
Transconjunctival fat removal at two week post-operative.